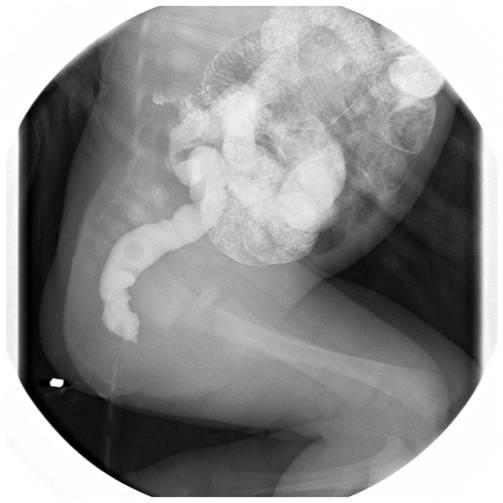
This 4-day-old female neonate had birth history of G2P2, gestational age 40 1/7 weeks, body weight 3432 gm, and delivered via vaginal delivery. The maternal history included: GDM(-), PIH(-), GBS(+), HbeAg(-), HbsAg(-). No abnormal finding was revealed by prenatal examinations. However, progressed abdominal distension was noted accompanied by vomiting several times. Feeding intolerance (10cc per 3 hours) was also noted since 2-day-old. She presented with heart murmur and cardiac sonography showed ventricular septal defect. Due to persistent abdomen distension, water-soluble contrast enema was arranged for suspect Hirschsprung's disease, showed small colon without obvious transition zone. Colon biopsy was done, reported no ganglion cell from anus till cecum and appendix. Then she received laparoscopic total colon resection + Duhamel ileal pull-through surgery for Hirschsprung's disease.
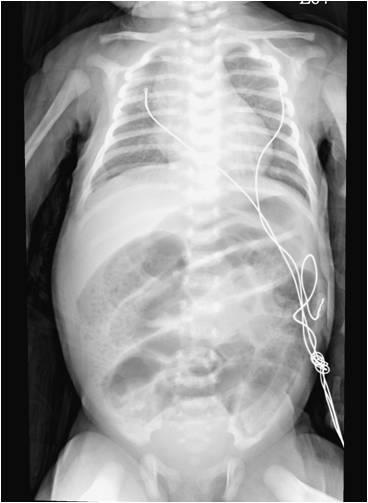
Fig. 1 (a) KUB showed distended intestine lumen. (b) Water-soluble contrast enema showed relative small colon without transition zone.