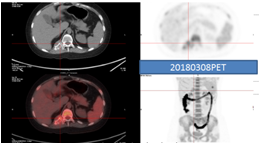
Alice (alias) was diagnosed to have juvenile idiopathic arthritis (JIA) when she was 12 years old. She received long-term treatment including steroid and low dose methotrexate since that time on. Her disease deteriorated 2 years later, combined with intermittent fever. Biological products including Tocilizumab (anti-IL6 monoclonal antibody) and Abatacept were ever used during April 2016 and December 2017 for her poor-controlled joint pain over bilateral knees, hands and wrists. In December 2017, cavernous sinus tumor was diagnosed with the presentation of right ptosis for 2 weeks. Based on the finding of a subpleural mass on CxR, chest CT was arranged which disclosed a 1.1cm pleural mass over right lower lung and lesion over right costovertebral junction. The result of biopsy on 2018/2/28 over right costovertebral junction was plasmacytoma. The following bone marrow aspiration and serum protein electrophoresis proved multiple myeloma. She received gamma knife radiosurgery on cavernous tumor on 2018/4/9. Meanwhile, chemotherapy for a total of 4 courses according to MM protocol had been administered since March 2018. Consolidated autologous peripheral blood stem cell transplant (PBSCT) was performed on 2018/6/12~13. Metabolic complete remission of multiple myeloma was achieved on the following PET-CT after treatment. Three years has passed since PBSCT, and she comes back to normal life. The result of her blood tests remains normal and her joint pain never recurred, in spite of mild wrist stiffness.